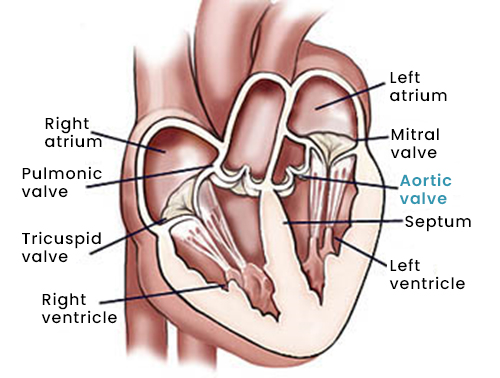
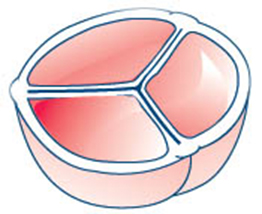
Instead of the normal three leaflets or cusps, the bicuspid aortic valve has only two. Without the third leaflet, the valve opening may not close completely and leak (regurgitant) or not open completely and become narrowed (stenotic) or leak.
In many cases, bicuspid aortic valves may function normally for several years without requiring treatment.
About 25 percent of patients with bicuspid aortic valves may have some enlargement of the aorta above the valve. If it is greatly dilated, the aorta is known as being aneurismal.
Acquired aortic valve disease
With acquired aortic valve conditions, changes occur in the structure of the valve. Acquired aortic valve conditions include:
Infective endocarditis is a bacterial infection of the valve, which is caused when bacteria enter your blood stream from the site of a remote infection and attach it to the surface of your heart valves. Dental cleaning or even minor infection, such as a tooth abscess, can cause severe bacterial endocarditis of the aortic valve.
Rheumatic fever is usually caused by a bacterial throat infection, such as strep throat. The valve itself is not infected in rheumatic fever, but antibodies developed by the body to fight infection react with the heart valves, causing stiffening and fusion of the leaflets of the aortic valve.
Aortic valve degeneration from wear and tear is another cause of acquired aortic valve disease. In many patients, the aortic valve leaflets degenerate and become calcified with time. This most frequently causes aortic stenosis, but may also cause aortic regurgitation. This is the most common cause of aortic stenosis in people over the age of 65.
Other causes of aortic valve disease include: rheumatoid arthritis, chronic inflammatory diseases, lupus, syphilis, hypertension, aortic aneurysms, connective tissue diseases, and less commonly, tumors, some types of drugs and radiation for cancers or lymphoma.
What are the symptoms of aortic valve disease?
Many patients with aortic valve disease are asymptomatic (have no symptoms), even when the stenosis (narrowing) or insufficiency (leak) are severe.
Initial symptoms of aortic valve disease usually include:
- Fatigue
- Easy tiring
- Loss of energy
- Swelling of the ankles
- Palpitations (extra or skipped heart beats)
More advanced symptoms may include:
- Shortness of breath
- Chest pain
- Dizziness or loss of consciousness
How is aortic valve disease diagnosed?
The diagnosis of aortic valve disease is made after your physician reviews your symptoms, performs a physical exam and listens for a murmur, and evaluates the results of your diagnostic tests.
During the physical exam, using a stethoscope, the doctor may hear a murmur, which represents turbulent blood flow across an abnormal valve.
The diagnosis of aortic valve disease is confirmed by a specialized heart ultrasound called an echocardiogram. The echocardiogram allows the doctor to visualize the heart valves and determine the severity and possible cause of the aortic valve disease.
In most patients, a standard transthoracic echocardiogram (in which a probe with gel is placed on the skin of the chest to transmit the images) is adequate to visualize the valve. The test may be combined with exercising or IV infusion of the drug allow the doctor to see the degree of stenosis more clearly.
Sometimes, a transesophageal echocardiogram (TEE – in which a probe is passed through the mouth into the esophagus) is necessary to more closely visualize the valve. A TEE is an outpatient procedure.
Procedure Details:
How is aortic valve disease treated?
If you do not have symptoms or heart damage, you will need to protect your valve from further damage by following precautions to reduce the risk of infective endocarditis, and you may need to take medications. In addition, surgery may be needed to treat your condition if you have symptoms, evidence of heart damage, or heart failure.
Aortic valve surgery
There are two types of aortic valve surgery: aortic valve repair and aortic valve replacement.
During aortic valve surgery, including aorta surgery, the aortic valve may be repaired or replaced. The results of your diagnostic tests, the structure of your heart, your age, the presence of other medical conditions and other factors will be considered to determine whether aortic valve repair or replacement is the best treatment approach for you.
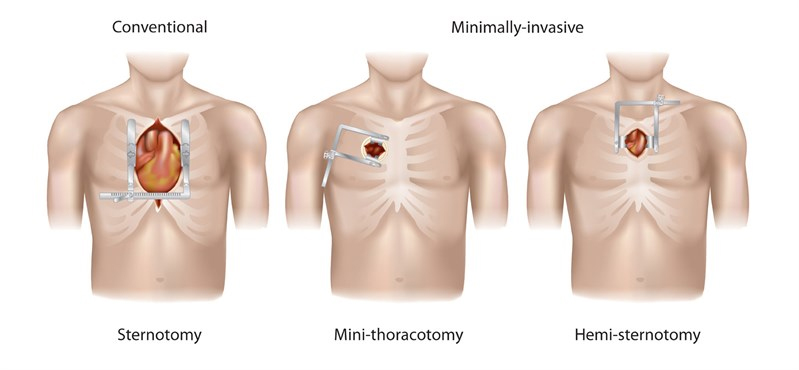
Aortic valve surgery can be performed using traditional heart valve surgery or minimally invasive approaches.
Traditional Aortic Valve Surgery
During traditional aortic valve surgery, a surgeon makes a 6- to 8-inch incision down the center of your sternum, and part or all of the sternum (breastbone) is divided to provide direct access to your heart. The surgeon then repairs or replaces your abnormal heart valve or valves.